

We focus on thorough examination – checking the overall health of your teeth and gums and taking x-rays when necessary. We teach personally maintenance & stress on routine cleanings, flossing, sealants, and fluoride which are all helpful in preventing dental disease. We are not only focused on the beauty of your smile, we're also concerned that the treatments are as painless as possible.
• Extraction of poor prognosis tooth and wisdom tooth removal
Need for tooth removal arises when :
- Your tooth is too damaged by a fracture or deep cavity to repair.
- You have a sizable infection that cannot be resolved by a root canal alone.
- You have teeth that are blocking other teeth from coming in. These may be extra teeth or baby teeth that have not fallen out yet.
- You are getting braces and need to get rid of a tooth that is crowding others.
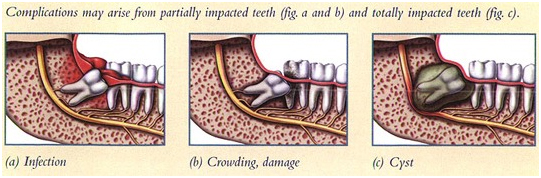
Wisdom teeth, which typically come in during your teens or twenties is usually the last teeth to erupt ,hence may get impacted—stuck underneath other teeth—when there is not enough space for it to come, which requires surgical removal and may need to be extracted if it is decayed, infected, or causing pain.

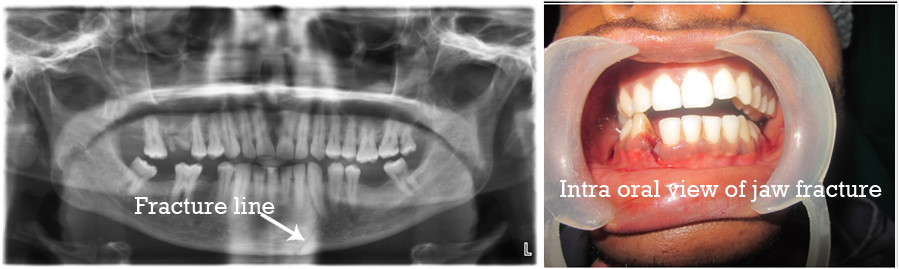
• Treatment of jaw fractures through imf and screw plating
A broken or dislocated jaw is an injury to the joints that join the upper and lower jawbone to the skull.
Broken, fractured, or dislocated jaws can create problems with eating and breathing. Immediate medical attention is required to minimize complications and accelerate healing.
Experiencing a facial injury is the primary cause of a broken or dislocated jaw. The jawbone extends from your chin to behind your ear.
Treatment for a jaw fracture depends on the extent of the injury. Clean breaks may heal on their own while your jaw is immobilized. Multiple fractures of the jawbone, as well as displaced breaks in which part of the bone is pushed off to one side, may be grounds for surgical repair with wiring or screw plating to promote healing.

• Oral Cyst and tumour removal
A cyst is a sac of tissue that has either fluid or soft material inside it.
Cysts can form in a wide range of tissues including in the face and mouth (including the jaws). Some can form next to or around teeth, which are called dental cysts.
Cysts are a reaction of the body to a condition and are usually relatively slow growing. They can be sterile or become infected.
Dental cysts can cause several problems but some remain undetected for months or even years. Many cause problems when:
- They become infected (causing pain and/or swelling);
- They slowly replace some bony tissue (they can weaken the jaws),
- They press against other teeth and structures;
- They prevent the normal function of the teeth and mouth tissues.
The treatment an oral and maxillofacial surgeon will recommend for a dental cyst depends on the location, type and size of cyst. Ideally, dentists or oral and maxillofacial surgeons want to remove the cyst tissue to:
- Examine it;
- Help the tissues to repair themselves
- To prevent another cyst from forming.
This is often done in combination with other treatment of the tooth (or teeth) associated with the cyst.
X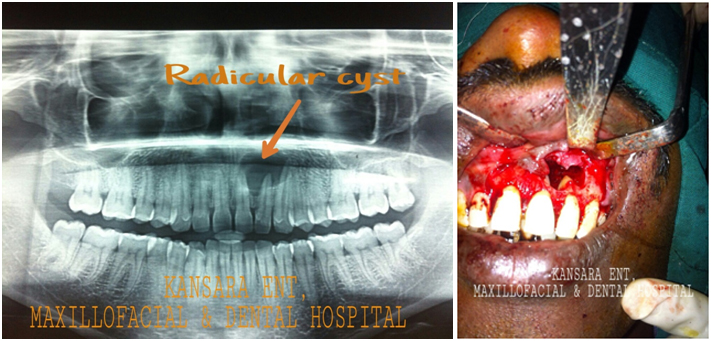

• Diagnosis and treatment of head & neck cancer
Cancer is defined as the uncontrollable growth of cells that invade and cause damage to surrounding tissue. Oral cancer appears as a growth or sore in the mouth that does not go away. Oral cancer, which includes cancers of the lips, tongue, cheeks, floor of the mouth, hard and soft palate, sinuses, and pharynx (throat), can be life threatening if not diagnosed and treated early.
The most common symptoms of oral cancer include:
- Swellings/thickenings, lumps or bumps, rough spots/crusts/or eroded areas on the lips, gums, or other areas inside the mouth
- The development of velvety white, red, or speckled (white and red) patches in the mouth
- Unexplained bleeding in the mouth
- Unexplained numbness, loss of feeling, or pain/tenderness in any area of the face, mouth, or neck
- Persistent sores on the face, neck, or mouth that bleed easily and do not heal within 2 weeks
- A soreness or feeling that something is caught in the back of the throat
- Difficulty chewing or swallowing, speaking, or moving the jaw or tongue
- Hoarseness, chronic sore throat, or change in voice
- Ear pain
- A change in the way your teeth or dentures fit together
Risk factors for the development of oral cancer include:
- Smoking. Cigarette, cigar, or pipe smokers are six times more likely than nonsmokers to develop oral cancers.
- Smokeless tobacco users. Users of dip, snuff, or chewing tobacco products are 50 times more likely to develop cancers of the cheek, gums, and lining of the lips.
- Excessive consumption of alcohol. Oral cancers are about six times more common in drinkers than in nondrinkers.
- Family history of cancer.
- Excessive sun exposure, especially at a young age.
As part of your routine dental examination, your dentist will conduct an oral cancer screening exam. More specifically, your dentist will feel for any lumps or irregular tissue changes in your neck, head, face, and oral cavity. If a suspicious lesion is seen biopsy test is necessary to confirm and detect oral cancer early, before it has had a chance to progress and spread.
• Surgical approach for reduced mouth opening, TMJ ankylosis and OSMF
Temporomandibular joint (TMJ) syndrome is a disorder of the jaw muscles and nerves caused by injury to the temporomandibular joint. The temporomandibular joint is the connection between the jawbone to the skull. The injured temporomandibular joint leads to pain with chewing, clicking, and popping of the jaw; swelling on the sides of the face; nerve inflammation; headaches; tooth grinding; Eustachian tube dysfunction; and sometimes dislocation of the temporomandibular joint.
The main symptom of TMJ syndrome is pain in the jaw joint. This joint is located just in front of the ear, and pain associated with TMJ syndrome may involve the face, eye, forehead, ear, or neck.
Signs and symptoms of TMJ syndrome include the following:
- Pain in the jaw, especially at the area of the joint
- Popping/clicking of the jaw
- Ear pain, or sounds of cracking in the ears
- Ringing or popping sounds in the ears (tinnitus) or a sense of fullness in the ears
- Headaches
- Locking or dislocation of the jaw (usually after widely yawning), referred to as lockjaw
Oral submucous fibrosis is a chronic debilitating disease of the oral cavity Oral submucous fibrosis results in marked rigidity and an eventual inability to open the mouth.[3, 4] The buccal mucosa is the most commonly involved site, but any part of the oral cavity can be involved.
The major causative factor is tobacco n areca nut chewing habits.
Symptoms of oral submucous fibrosis include the following[3] :
- Progressive inability to open the mouth (trismus) due to oral fibrosis and scarring
- Oral pain and a burning sensation upon consumption of spicy foodstuffs
- Increased salivation
- Change of gustatory sensation
- Hearing loss due to stenosis of the eustachian tubes
- Dryness of the mouth
- Nasal tonality to the voice
- Dysphagia to solids (if the esophagus is involved)
- Impaired mouth movements (eg, eating, whistling, blowing, sucking)
The treatment of patients with oral submucous fibrosis depends on the degree of clinical involvement. If the disease is detected at a very early stage, cessation of the habit is sufficient.
Medical treatment is symptomatic and predominantly aimed at improving mouth movements. Severe cases can be treated with surgical approach.
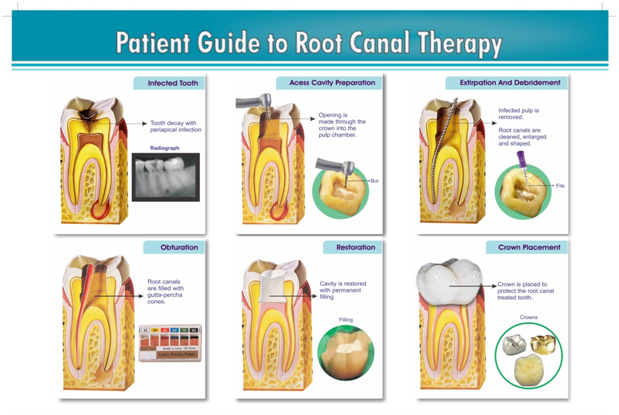
• Root canal treatments
Root canal treatment is the removal of the tooth's pulp, a small, thread-like tissue in the center of the tooth. Once the damaged, diseased or dead pulp is removed, the remaining space is cleaned, shaped and filled. This procedure seals off the root canal. Years ago, teeth with diseased or injured pulps were removed. Today, root canal treatment saves many teeth that would otherwise be lost.
The most common causes of pulp damage or death are:
- A cracked tooth
- A deep cavity
- An injury to a tooth, such as a severe knock to the tooth, either recent or in the past.
Once the pulp is infected or dead, if left untreated, pus can build up at the root tip in the jawbone, forming an abscess. An abscess can destroy the bone surrounding the tooth and cause pain.

• Teeth whitening
We all want our smile to be dazzling, and teeth whitening is becoming a very popular. Teeth whitening allows us to remove or reduce stains on your teeth, giving them a brighter, more attractive appearance and can help give you the smile of your dreams. Our teeth develop stains because the enamel becomes more porous as we age, and gradually becomes darker. Acidic foods and drinks -- such as diet soda -- makes the enamel even more porous, and leave it vulnerable to stains. Tobacco, red wine, coffee and tea are the most likely to leave those ugly yellow stains on our teeth.

• Aesthetic smile designing / veneers/ laminates
Dental veneers (sometimes called porcelain veneers or dental porcelain laminates) are wafer-thin, custom-made shells of tooth-colored materials designed to cover the front surface of teeth to improve your appearance. These shells are bonded to the front of the teeth changing their color, shape, size, or length.
Veneers are routinely used to fix:
- Teeth that are discolored -- either because of root canal treatment; stains from tetracycline or other drugs, excessive fluoride or other causes; or the presence of large resin fillings that have discolored the tooth
- Teeth that are worn down
- Teeth that are chipped or broken
- Teeth that are misaligned, uneven, or irregularly shaped (for example, have craters or bulges in them)
- Teeth with gaps between them (to close the space between these teeth)

• Dental jewellery
Dental Jewellery is a brilliant way to add sparkles to your smile and stand out of the crowd.
During a painless procedure, we fix a jewel on your tooth surface. The jewel does not damage tooth tissues and has no side effects - except for the increased charm of your smile! Call it an oral fashion statement to stand out among ordinary mortals or simply an effort to blend in with the bold and the beautiful.
If somebody thinks he or she was better off without Dental Jewellery, it can be easily removed without any side effects on the dental tooth structure as the procedure is non-invasive. What's more, tooth jewellery can be fixed again at a later stage.

• Teeth cleaning/scaling
Every day our mouths are full of sugary, sticky food. Bacteria from that food causes a biofilm called plaque. If not removed from the teeth, plaque hardens into dental calculus (also called tartar). Calculus builds up between teeth and between your teeth and gums, |
|
and can cause gums to become inflamed or infected. This in turn can lead to gum disease which has been linked to a host of other medical issues, including diabetes, dementia, and heart disease. |
|
Why Would I Need Deep Cleaning?
While most people need regular cleanings, some have so much calculus built up that they need extra care. This additional buildup may be caused by age, hereditary factors, or poor oral hygiene (which includes skipping regular cleanings). If your dentist recommends deep cleaning, it’s very important to follow through, as you likely have the beginnings of gum disease. Deep cleaning will remove calculus from above and below your gum line, and get rid of rough places where bacteria collects.

• Periodontal therapy
Gum disease is an infection of the tissues that surround and support your teeth. It is a major cause of tooth loss in adults. Because gum disease is usually painless, you may not know you have it. Also referred to as periodontal disease, gum disease is caused by plaque, the sticky film of bacteria that is constantly forming on our teeth.
Here are some warning signs that can signal a problem:
• gums that bleed easily
• red, swollen, tender gums
• gums that have pulled away from the teeth
• persistent bad breath or bad taste
• permanent teeth that are loose or separating
• any change in the way your teeth fit together when you bite
• any change in the fit of partial dentures
Some factors increase the risk of developing gum disease. They are:
• poor oral hygiene
• smoking or chewing tobacco
• genetics
• crooked teeth that are hard to keep clean
• pregnancy
• diabetes
• medications, including steroids, certain types of anti-epilepsy drugs, cancer therapy drugs, some calcium channel blockers and oral contraceptives
See your dentist if you suspect you have gum disease because the sooner you treat it the better.
• Non-Surgical Treatments
• Gum Graft Surgery
• Laser Treatment
• Regenerative Procedures
• Dental Crown Lengthening
• Dental Implants
• Pocket Reduction Procedures
• Plastic Surgery Procedures
• Replacing missing teeth by Denture, Caps & Bridges and Dental Implants.
Replacing missing teeth involves using dentures, bridges and implants to improve your appearance and dental health.
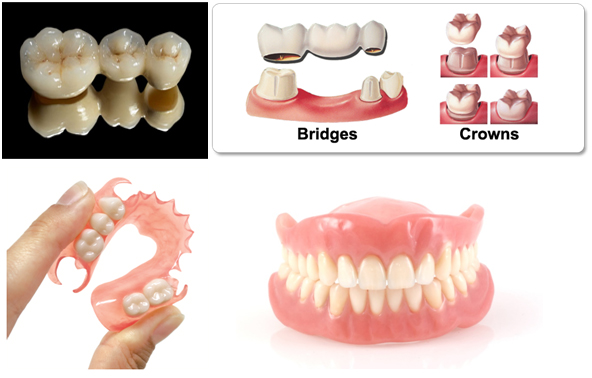
Various treatment options to replace missing teeth are:
- Dentures – removable or tooth supported acrylic or metal frameworks that carry artificial teeth.
- Bridges – artificial teeth that are fixed onto adjacent natural teeth.
- Dental implants – metal 'screws' are placed in your jawbone, and dentures, crowns or bridges are clipped or screwed on top of them.
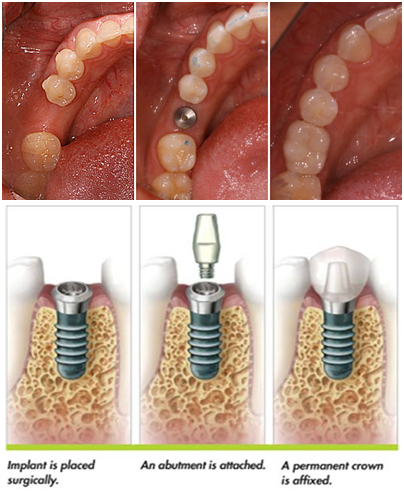
Dental Implants have changed the face of dentistry
Dental implants are replacement tooth roots. Implants provide a strong foundation for fixed (permanent) or removable replacement teeth that are made to match your natural teeth without taking support or grinding your adjacent natural teeth. .
Like tooth roots, dental implants are secured in the jawbone and are not visible once surgically placed.
The most appropriate treatment for you will depend on the number of teeth you have missing. It will also depend on where teeth are missing in your mouth and the condition of any remaining teeth. Your dentist will help you decide which option is best for you.
• Orthodontic treatment
orthodontic treatment is a way of straightening or moving teeth, to improve the appearance of the teeth and how they work. It can also help to look after the long-term health of your teeth, gums and jaw joints, by spreading the biting pressure over all your teeth.
Crooked teeth and teeth that do not fit together correctly are harder to keep clean, are at risk of being lost early due to tooth decay and periodontal disease, and cause extra stress on the chewing muscles.

• Paediatric dental treatments
Give your little ones the smile they deserve. Correct oral habits and methods for oral hygiene are very important to shape every young mind so that your child has perfect set of teeth.
At Kansara Hospital our young patients are treated with fun and love making their experience fearless and enjoyable.

| • Consulting rooms with minor and major operation theatre. |
| • 3 indoor patients rooms facilitated with Ac, TV & refrigerator. |
| • Audiology comprising of Pure tone audiology, impedance audiology and guidance for cochlear implant surgery. |
| • Speech therapy |
| • Zeiss microscope for microsurgery |
| • Karl storz endoscopy unit |
| • Xomed microdebrider |
| • Bayne air micro drill |
| • Radio frequency cautery |
| • Satellac P5 scaler |
| • Kodak RVG ( Digital Xray) |